We include products in articles we think are useful for our readers. If you buy products or services through links on our website, we may earn a small commission.
Does Red Meat Cause Cancer? The Science Says No

Does red meat cause cancer? If you’ve been paying attention to mainstream nutritional dogma over the last half century, you probably think it does.
But the fact is, there are NO control trials linking meat to cancer. And even when considering the few observational (epidemiological) studies that our guidelines for limiting meat are based on, there is no significant evidence supporting the link between red meat and cancer. The few insignificant correlations have been thoroughly corrected by newer, high-quality review studies.
Leaving aside the ideological question of why some anti-meat studies make headlines while other studies supporting the healthiness of meat get suppressed, let’s take a close look at the major studies exploring the possible links between meat and cancer.
We’ll let the science speak for itself.
Table of Contents
Does Red Meat Cause Cancer? Collected Research
Let’s turn to the major studies exploring the relationship, or, more accurately, the absence of a relationship, between red meat and cancer.
Unprocessed Red Meat Consumption and Processed Meat Consumption – Johnston et al.
The 2019 NutriRECS study is one the most comprehensive reviews of the evidence linking meat consumption with cancer to date. Researchers described the purpose of the study as follows:
 The authors state, “Contemporary dietary guidelines recommend limiting consumption of unprocessed red meat and processed meat. For example, the 2015–2020 Dietary Guidelines for Americans recommend limiting red meat intake…The World Health Organization International Agency for Research on Cancer has indicated that consumption of red meat is “probably carcinogenic” to humans, whereas processed meat is considered “carcinogenic” to humans (4).
The authors state, “Contemporary dietary guidelines recommend limiting consumption of unprocessed red meat and processed meat. For example, the 2015–2020 Dietary Guidelines for Americans recommend limiting red meat intake…The World Health Organization International Agency for Research on Cancer has indicated that consumption of red meat is “probably carcinogenic” to humans, whereas processed meat is considered “carcinogenic” to humans (4).
However, the researchers found that “These recommendations are, however, primarily based on observational studies that are at high risk for confounding and thus are limited in establishing causal inferences, nor do they report the absolute magnitude of any possible effects. Furthermore, the organizations that produce guidelines did not conduct or access rigorous systematic reviews of the evidence, were limited in addressing conflicts of interest, and did not explicitly address population values and preferences, raising questions regarding adherence to guideline standards for trustworthiness (5–9).”
Results for fresh red meat
The results of this analysis for consuming red meat with “17 cohorts with 2.2 million participants provided low-certainty evidence that decreasing unprocessed red meat intake may result in a very small reduction of overall lifetime cancer mortality (7 fewer events per 1000 persons with a decrease of 3 servings/wk), with no statistically significant differences for 8 additional cancer outcomes (prostate cancer mortality and the incidence of overall, breast, colorectal, esophageal, gastric, pancreatic, and prostate cancer) (13)
Results for processed meat
“For cohort studies addressing adverse cancer outcomes (31 cohorts with 3.5 million participants providing data for our dose–response analysis), we also found low- to very low-certainty evidence that a decreased intake of processed meat was associated with a very small absolute risk reduction in overall lifetime cancer mortality; prostate cancer mortality; and the incidence of esophageal, colorectal, and breast cancer (range, 1 fewer to 8 fewer events per 1000 persons with a decrease of 3 servings/wk), with no statistically significant differences in incidence or mortality for 12 additional cancer outcomes (colorectal, gastric, and pancreatic cancer mortality; overall, endometrial, gastric, hepatic, small intestinal, oral, ovarian, pancreatic, and prostate cancer incidence)”
Final Recommendations
Based on the above analysis the researchers recommend continuing to eat both fresh red meat and processed meats.
A Review and Meta-Analysis of Prospective studies of red and processed meat, meat cooking methods, heme iron, heterocyclic amines and prostate cancer – Bylsma et al.

In the above analysis from 2015 red meat was shown to have no relationship with colon cancer when including consideration of cooking methods and other mitigating factors.
Note that the carcinogenic compounds in fresh red meat occur from cooking, but this study found that they had no effect on cancer risk [5].
Association Between Red Meat Consumption and Colon Cancer – Turner et al.
This 2017 review of numerous studies found that “there is currently insufficient evidence to confirm a mechanistic link between the intake of red meat as part of a healthy dietary pattern and colorectal cancer risk.”
The study authors came to this conclusion because, as they observed, “Most studies used levels of meat or meat components well in excess of those found in human diets. Although many of the experiments used semi-purified diets designed to mimic the nutrient loads in current westernized diets, most did not include potential biologically active protective compounds present in whole foods” [11].
Meta-analysis of prospective studies of red meat consumption and colorectal cancer – Alexander et al.
Similarly, this 2011 analysis of 25 studies found insufficient evidence to support an association between red meat and colon cancer–the most common cancer attributed to eating red meat [16].
Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence: A Systematic Review and Meta-analysis of Cohort Studies – Han et al.
This major review study of 73 other studies concluded, “The possible absolute effects of red and processed meat consumption on cancer mortality and incidence are very small, and the certainty of evidence is low to very low” [4].
Common dietary patterns and risk of cancer of the colon rectum – Jauregui et al.
This 2018 study found no difference in colorectal cancer rates between participants who consumed red meat, and vegetarians [5].
If red meat were a carcinogen, then wouldn’t you expect the non-meat diet to have some positive effect?
Lack of Association between Red Meat Consumption and Positive Fecal Immunochemical Colorectal Cancer Screening Test – Pramul et al.
This large-scale randomized control trial with 1060 people between the ages of forty-seven and seventy-four found no association between meat consumption and carcinogenic faecal biomarkers.
The researchers conclude: ‘No significant associations were noted with any of the variables, except for being aged 60–74 years.
Suprisingly for some, but not for carnivore diet proponents like Dr. Kiltz, “Borderline significance was observed for high consumption of vegetables.”
When considering the presence of plant toxins and the myth-busting research showing that insoluble fiber in vegetables promotes IBS and intestinal polyps, this finding makes perfect sense.
Effect of Meat – Parnaud et al.

In this classic study from 1998, rats that were fed a bacon-based diet had the lowest rates of colon cancer.
Eating bacon even showed protective effects for rats who were dosed with a compound meant to promote colon cancer. While rats fed a “balanced” diet of “chow” did not have these effects.
Diet, obesity, and colorectal carcinoma risk – Alsheridah et al.
In this 2018 study out of Kuwait that did show a small correlation between red meat consumption and colorectal cancer, those who ate red meat were less likely to have type 2 diabetes.
Meat intake and recurrence of colorectal adenomas – Mathew et al.
This 2004 study found that for people with precancerous colon polyps, reducing red meat did not decrease the risk of recurrence [6].
Meat intake and cause-specific mortality – Lee et al.

In this review of 8 Asian studies surveying of 300,000 participants for periods from 6 to 15 years “Red meat intake was inversely associated with CVD mortality in men and with cancer mortality in women in Asian countries” [8].
Multiple risk factor intervention trial –
In this classic study spanning 9 years with data from 361,000 participants, the group that lowered saturated fat died at higher rates.
Tragically, at the 16-year follow-up, participants in this group had 20% higher rates of lung cancer even when they quit smoking [8].
Saturated fat is a significant variable because it is the component of meat that was first demonized over 60 years ago by Ansel Keys infamous seven countries study. This study falsely puts the bullseye on meat as the number one public health enemy.
In conclusion, both the vegetarians and the nonvegetarians in the EPIC-Oxford study have a low total cancer incidence compared with the national average. The incidence of all malignant neoplasms combined was lower among vegetarians and fish eaters than among meat eaters, but the incidence of colorectal cancer was significantly higher among vegetarians than among nonvegetarians. (Other articles in this supplement to the Journal include references 24–50.)
Key Factors that Meat Research Misses
The large scale population studies that diet guidelines are based on cannot, or do not, control for many factors that might increase the risk of colorectal cancer independent of red meat consumption.
Furthermore, studies show that the number one correlation with meat consumption is lifestyle behavior that includes physical inactivity, smoking habits, and alcohol consumption. This tells us much more about the promotion of plant based diets as healthy than it does about the healthiness of meat.
But even studies that attempt to control for factors like heredity, smoking, alcohol use, and exercise all miss the presence of seed “vegetable oil” in the diet.
Seed Oil as Carcinogen
Dietary nutrition thought leaders like Mark Sisson point out that the presence of seed oils may be the most important factor when determining whether or not meat is carcinogenic in the colon.
In fresh red meat, heme iron is the compound that is most often identified as carcinogenic. However, it is essentially only carcinogenic when combined with omega-6 fatty acids, specifically linoleic acid.
 In the above study, feeding heme iron to rats promoted colon cancer only when fed alongside high-linoleic acid safflower oil.
In the above study, feeding heme iron to rats promoted colon cancer only when fed alongside high-linoleic acid safflower oil.
When heme iron was fed alongside olive oil, which is higher in SFAs (saturated fatty acids) more stable MUFAs (monounsaturated fatty acids), the olive oil prevented colon carcinogenesis [10].
In this 2004 study, meats containing medium to high amounts of heme—beef and beef blood sausage—were found to promote carcinogenic conditions in the colon when combined with corn and soybean oil rich in omega-6 linoleic acid [11].
In this study from 2015, mice were split into three groups.
The first group was fed heme iron and omega-6 PUFA from safflower oil.
A second group was fed heme iron with omega-3 PUFA from fish oil.
A third group was fed heme iron with saturated fat and zero PUFA from fully hydrogenated coconut oil.
To find out how carcinogenic each feeding regimen was, the researchers looked at the effects of the animals’ “fecal water” on colon cells.
Both PUFA groups showed numerous markers of carcinogenesis and lipid oxidation. In short, the fecal water of PUFA and iron fed mice was toxic to colonic epithelial cells.
The fecal water from mice fed saturated fat, and heme iron showed no markers of carcinogenesis or lipid oxidation.
Sugar as a Carcinogen
The average American gets around 50-60% of their calories from carbohydrates and 16% from added sugars alone. [81]
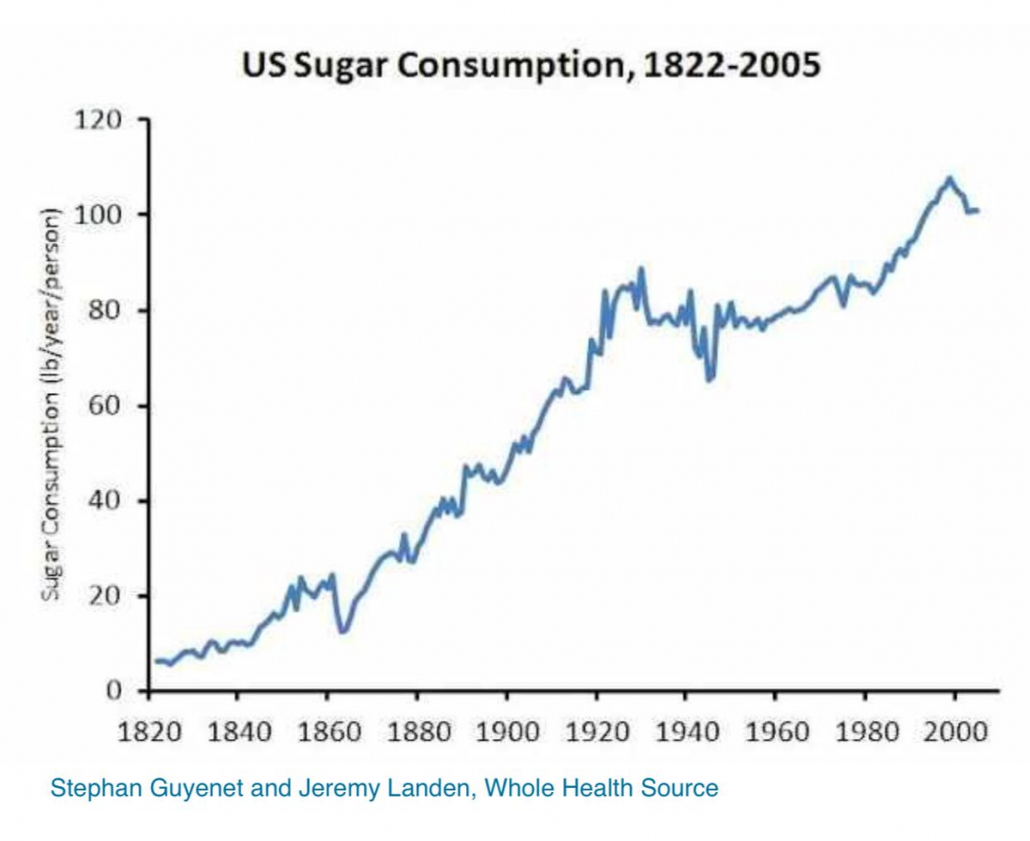
A 2019 study links drinking just a small 100 ml glass of a sugary drink per day–only a third of a typical can of soda–to an 18% increase in overall cancer risk, and a 22% increase in risk for breast cancer.
Not surprisingly, the increased risk of cancer in consuming sugary drinks was observed even among consumers of pure fruit juice. Mathilde Touvier, the research director of the Nutritional Epidemiology Research Team of the National Health and Medical Research Institute at the Paris 13 University, states, “What we observed was that the main driver of the association seems to be really the sugar contained in these sugary drinks.”
The cells of many human cancers depend on blood sugar to grow and multiply and even develop mutations that allow them to increase the energy they get from insulin. Researchers believe that many pre-cancerous cells would never become malignant tumors if they weren’t being fueled by sugar.
Where Did The Meat-Cancer Connection Come From?
Since at least 1975, scientists have been attempting to link the consumption of red meat and cancer–especially colorectal cancer.
The current WHO position that meat may be carcinogenic comes primarily from what is known as the IARC study.
In this study, a group of researchers concluded (without consensus) that: ‘”After thoroughly reviewing the accumulated scientific literature, a Working Group of 22 experts from 10 countries convened by the IARC Monographs Programme classified the consumption of red meat as probably carcinogenic to humans (Group 2A), based on limited evidence that the consumption of red meat causes cancer in humans and strong mechanistic evidence supporting a carcinogenic effect. This association was observed mainly for colorectal cancer, but associations were also seen for pancreatic cancer and prostate cancer.”
This is remarkably misleading for numerous reasons
- The researchers say they considered 800 studies but actually reviewed only 14
- None of the studies reviewed were controlled trials. They were all unreliable epidemiological (observational) studies that, as a rule, cannot attribute causation. These studies are based on lifestyle questionnaires mailed to participants, leaving them highly prone to faulty reporting
- Despite protest from Dr. David Klurfeld, the study omitted two controlled studies looking at breast and colon cancer where the elimination of red meat and increase in fruits and grains did not lower risk of cancer
- Of the 14 observational studies, only 6 showed a positive correlation between eating meat and cancer risk
- Of those six positive studies, only 1 showed a ‘significant’ correlation of only 1.85 positive association.
To put these findings in perspective, the positive observational correlation between smoking and cancer is 2000%. For meat it’s 47%.
It’s also worth highlighting how low observational studies sit on the hierarchy of evidence. They are intended to make a case for further controlled studies, and not to be used for the basis of definitive claims.
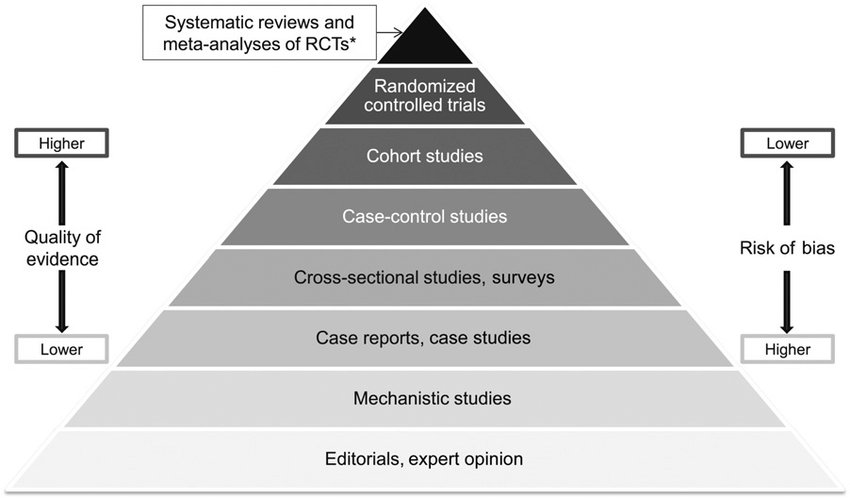
Study designs in ascending levels of the pyramid generally exhibit increased quality of evidence and reduced risk of bias. Confidence in causal relations increases at the upper levels. *Meta-analyses and systematic reviews of observational studies and mechanistic studies are also possible. RCT, randomized controlled trial. Source American Journal of Clinical Nutrition
How Studies are Fudged and Dogma is Made
At this point, you might be wondering who is behind these anti-meat guidelines and their misrepresentation to the public. For the first time in decades, we don’t have to speculate, we can hear it straight from the top.
Dr. David Klurfeld, a highly respected researcher and member of the working group of the World Health Organization that decided meat causes cancer in 2015, has spoken out.
Dr. Klurfeld was strongly opposed to this designation and called it the most frustrating professional experience of his life.
Not your standard low-level whistleblower, Dr. Klurfeld has been the National Program Leader for Human Nutrition in the Agricultural Research Service of the USDA since 2004. You can find his peer-reviewed article defending meat titled “What is the role of meat in a healthy diet” here.
Below you can hear Dr. Klurfeld speak about meat not causing cancer and the ideologically motivated vegan researchers behind the WHO guidelines.
Meat and Colorectal Cancer in UK Biobank: A Prospective Study
This 2019 study linking meat and colon cancer got a lot of attention. Let’s examine it to see just how the “meat causes cancer” sausage is made.

Below is the press release from the study that shows how it was broadcast to the public:
The reporting on this study is a prime example of misrepresentation, vilification, and fear-mongering.
The press release begins: “Scientists have shown that people eating around 76g of red and processed meat a day– which is roughly in line with government recommendations– still had a 20% higher chance of developing bowel cancer than those who only ate about 21g a day” [2].
20% sounds pretty high, but what the reporters omit is that it’s a relative 20% increase in risk, not an absolute 20% increase.
The study participants began with a 0.5% risk of colorectal cancer. Those who ate the most processed and red meat showed a risk increase to 0.6%. Since the difference between 0.5% and 0.6% is 20%, the researchers came up with a 20% “relative” increase in risk,
For the sake of argument, let’s assume that the self-reported surveys that this study relied on were completely accurate. That they accounted for all other possible confounding factors like exercise, heredity, smoking, alcohol use, soft drink consumption, time spent sitting at work etc. (which would be impossible). Would you still cut out the pleasure of bacon, let alone the rich matrix of complete proteins, B vitamins, zinc, and meat-specific nutrients found in fresh red meat, to reduce your risk of colon cancer by 0.1%?
And remember that this 0.1% isn’t even causal. It’s only a correlation.
But what if all you read was the headline of the press release? This is how the so-called science linking meat with cancer has been conducted and disseminated for the last century.
What Else Was Omitted?
Not only are the statistics in these studies presented in a misleading way, key details are omitted.
Only Processed Meat was Correlated with Increased Risk
Also not mentioned in the press release on the study is that there was NO link between unprocessed red meat and colon cancer. There was only a 0.1% link between processed meat and colon cancer.
Yet the study is still sold to the public as showing that “red and processed meat eaters” are at greater risk.
Colon Cancer Risk for Women was Unaffected by Red and Processed Meat
In another twist, red meat, whether processed or fresh, showed no significant association with colorectal cancer in women.
So the title of the press release, “Even moderate red and processed meat eaters at risk of bowel cancer,” is more than misleading and grossly overstated. When it comes to half the population, it’s an outright lie.
But don’t just blame the press release–it’s not even mentioned in the abstract. To get the real story you, your mom, sister, wife, etc, and every journalist have to read the fine print.
Why would the study authors hide the finding that red meat did not increase the risk of colon cancer in women?
Because doing so would have completely undermined their “story” that red meat was a carcinogen. A story that they had spent over five years and hundreds of thousands of dollars trying to prove.
Though there are real physiological differences between men and women, these were not what the study was looking for.
The Nitrate/Nitrite Fallacy
Now let’s dig a bit deeper into one of the so-called “mechanistic” pathways that get meat labeled as “possibly carcinogenic”- nitrates and nitrites.
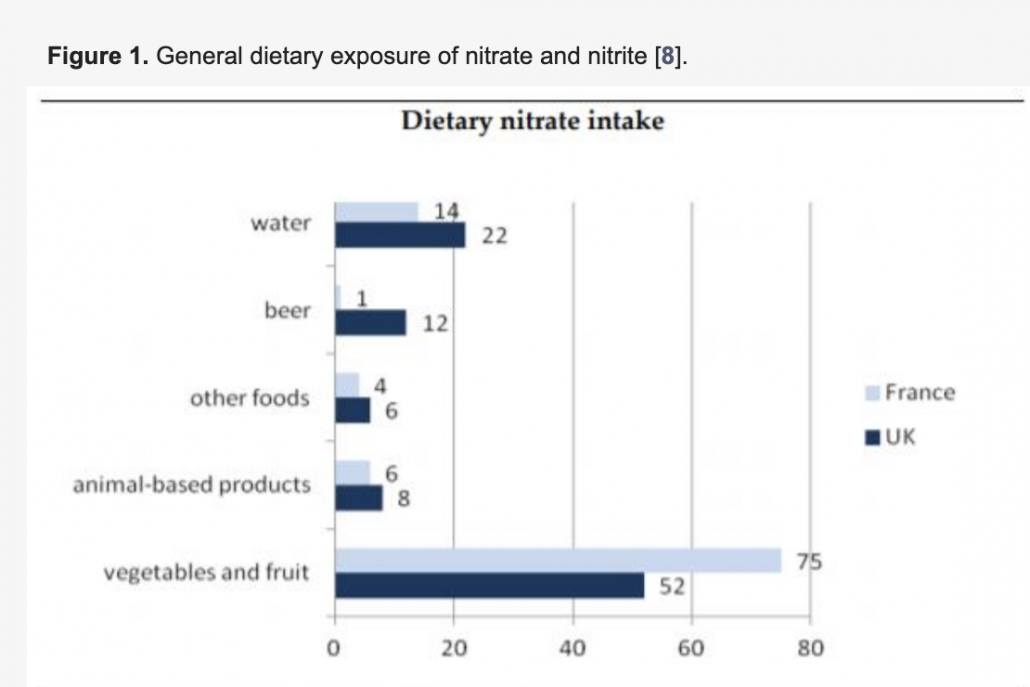
Interestingly, these compounds are found in much greater abundance in plants than in processed and cured meats. They supply plants with the nitrogen that they need to grow.
In fact, vegetables are by far the greatest source of nitrates in our diet.
Veggies account for at least 85% of the nitrates humans consume. Cured processed meats account for around only 5% of nitrate consumption.
Nitrates are essentially harmless, but they can be converted into nitrites by the microbes in our mouths. When swallowed, these nitrites can react in the acidic environment in our stomachs to become nitrosamines. Some nitrosamines have been shown to be carcinogenic.
If you’re worried about nitrosamine formation when eating animal or plant sources research shows that using an anti-bacterial mouthwash can significantly reduce the oral creation of nitrites.
It’s also important to note that nitrates play very important roles in the body. In 1998 US scientists won the Nobel prize for discovering the roles of nitric oxide in the cardiovascular system. Your body creates this gas from nitrates in your food.
The nitric oxide from nitrates dilates blood vessels, lowers blood pressure, and protects against infections. When your ability to produce nitric oxide is inhibited, you have a higher risk of heart disease, diabetes, and erectile dysfunction.
So why is processed meat considered carcinogenic and not vegetables? The main theory follows that vegetables have antioxidants that protect against the effects of nitrites.
But again, let’s note that there was only that 0.1% link between processed meat and colon cancer (in men, but not women) due to all three potentially carcinogenic pathways listed above. So are nitrates really a risk? And is the insignificant, potential (but not causal) risk factor of nitrates a reason to eliminate these nutrient-rich processed meats like bacon?
When looking at the evidence, it is even more likely that nitrates are good, and avoiding them as part of a dense whole foods nutrient matrix in meat results in net negative health outcomes.
The Methionine Cancer Link
There is one more link that researchers make between meat and cancer, and it has to do with an amino acid called methionine that meat is high in.
However, when studies look at methionine, they find that in order to increase base levels of homocysteine (an amino acid synthesized from methionine and associated with disease), you need a very high dose of pure methionine. This comes to around 500% of the normal daily intake [12].
Normal methionine doses, as you would get from a keto diet and even a carnivore diet, do not increase base levels of homocysteine [7][8].
Put simply; there is no convincing evidence showing that for healthy people, a diet high in muscle meat increases base levels of homocysteine.
If you’re worried about methionine, one approach is to drink more bone broth rich in amino acids like glycine, which have been shown to mitigate the effects of methionine.
Does Red Meat Cause Cancer? The Bottomline
Based on all available evidence, it does not appear that red meat, whether fresh or processed, causes cancer.
However, when the heme iron from red meat is combined with seed oils, it may have carcinogenic properties.
When consumed as part of a low PUFA diet, red meat is likely very beneficial. Fatty cuts of steak like ribeye are among the most nutrient-dense foods on earth.
Red meat offers an abundance of bioavailable and meat-specific nutrients, is highly satiating, and is associated with numerous markers of health, fertility, and longevity [17][18].
Humans Evolved Consuming a Diet of Mostly Meat
Furthermore, there is emerging research showing that modern humans are nearly physiologically identical to that of our caveman ancestors.
For nearly 2 million years, our ancestors evolved on a diet of mostly fatty red meat [22].
Eat Meat to Live Longer
Not only does the evidence suggest that red meat does not cause cancer, but numerous other studies have also found that total meat consumption correlates with greater life expectancy. This finding is independent of total caloric intake, economic status, urban advantages, and obesity [16].